Managing healthcare finances is a high-stake balancing act. On one side, hospitals and providers struggle with shrinking margins, rising costs, and complex reimbursement structures. On the other, an ocean of untapped financial data holds the key to smarter decision-making and optimized revenue. So, what if financial analytics could be the game-changer your organization needs?
The Financial Pressures on Healthcare Organizations
The financial landscape of healthcare is more challenging than ever. With increasing regulatory pressures, administrative burdens, and fluctuating payer reimbursements, hospitals and healthcare providers face mounting financial instability. According to the American Hospital Association (AHA), in 2022 alone, hospitals faced a staggering $130 billion in underpayments from Medicare and Medicaid. Add rising labor, drug, and medical supply costs into the mix, and the financial strain becomes overwhelming.
Yet, many healthcare organizations still rely on outdated financial management methods—manual spreadsheets, disconnected data sources, and retrospective reporting—that limit agility and efficiency. To remain competitive, hospitals must embrace data-driven financial analytics to optimize revenue cycles, reduce inefficiencies, and ensure compliance.
Key Financial Challenges in Healthcare
If your organization is still relying on traditional financial processes, you’re likely leaving money on the table. Below are some of the most pressing financial challenges in healthcare today:
Revenue Leakage
Revenue loss due to claim denials, coding errors, and reimbursement delays is a significant issue. While many denials are preventable, a large percentage are never resubmitted, resulting in substantial lost revenue.
Rising Operational Costs
From increasing labor expenses to supply chain disruptions, financial strain is mounting. Without real-time financial visibility, healthcare organizations struggle to control costs effectively.
Lack of Predictive Insights
Without robust analytics, financial teams operate reactively rather than proactively. This lack of foresight hinders strategic decision-making, making it difficult to optimize budget planning and mitigate financial risks before they escalate.
Manual & Time-Consuming Reporting
Spreadsheets and manual data entry not only slow down operations but also increase the risk of errors. Inefficient reporting methods lead to administrative burdens and data discrepancies that impact financial decision-making.
Compliance & Regulatory Risks
Navigating complex regulations such as CMS, HIPAA, and FHIR requires strict adherence to avoid costly penalties. Non-compliance can lead to reimbursement denials, audits, and financial setbacks.
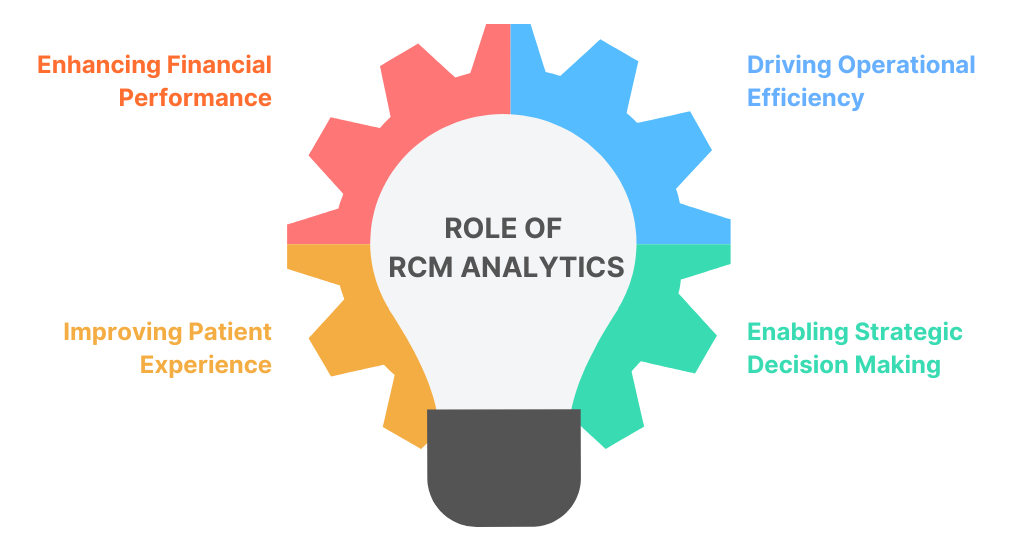
How Financial Analytics is Transforming Healthcare Finance
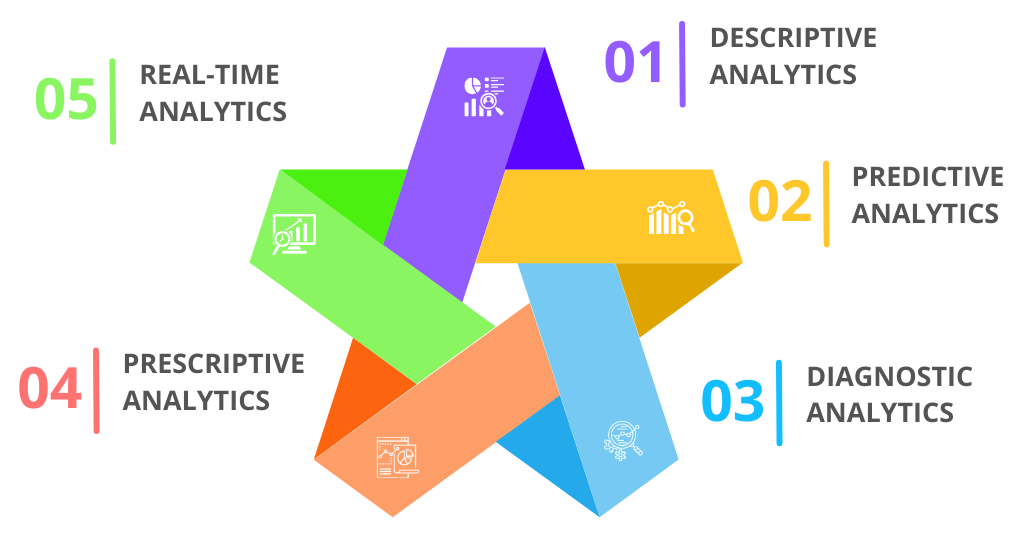
Financial analytics in healthcare isn’t just about crunching numbers—it’s about turning data into actionable insights that drive profitability and efficiency. Here’s how healthcare organizations can leverage financial analytics to stay ahead:
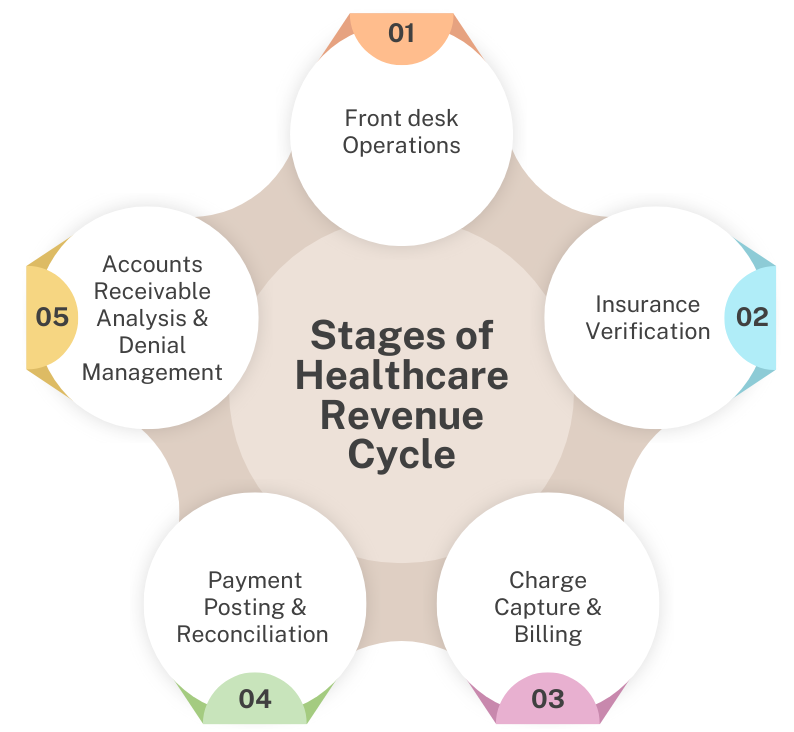
Proactively Prevent Revenue Loss
Claims denials due to coding errors, missing documentation, or payer discrepancies often go unaddressed. Financial analytics in healthcare helps identify high-risk claims before submission, detect underpayments, and recover lost revenue. With predictive modeling and optimized billing workflows, healthcare organizations can streamline reimbursements and maintain steady cash flow.
Gain Real-Time Financial Visibility
A dynamic financial dashboard provides real-time insights into cash flow, reimbursements, and cost-saving opportunities. AI-driven predictive forecasting enables organizations to anticipate financial trends, optimize budgets, and make informed staffing decisions that enhance operational efficiency.
Smarter Budgeting & Financial Planning
With accurate forecasting, finance teams can proactively manage cash flow fluctuations, track account receivables, and allocate resources effectively. This ensures financial stability and long-term growth with confidence.
Turn Compliance into a Strategic Advantage
Healthcare financial analytics automates reporting, detects billing anomalies, and ensures timely reimbursements that align with evolving regulations. By leveraging real-time insights, healthcare providers can reduce audit risks, prevent revenue leakage, and enhance overall financial efficiency.
How VNB Health is Driving Financial Success
In today’s fast-changing healthcare environment, financial stability depends on data-driven decision-making. Traditional financial management methods are no longer enough. VNB Health’s Financial Analytics Solution empowers healthcare organizations with cutting-edge tools to optimize revenue cycles, reduce inefficiencies, and ensure seamless compliance.
Our comprehensive financial dashboards, predictive analytics, and automated reporting tools provide CFOs and financial teams with real-time insights to make informed, strategic decisions. From detailed Profit & Loss Reports and Balance Sheet Reports to real-time AR tracking, our solutions help healthcare providers improve cash flow, mitigate risks, and achieve long-term financial success.
Ready to transform your healthcare finances? Explore VNB Health’s Financial Analytics solution today!