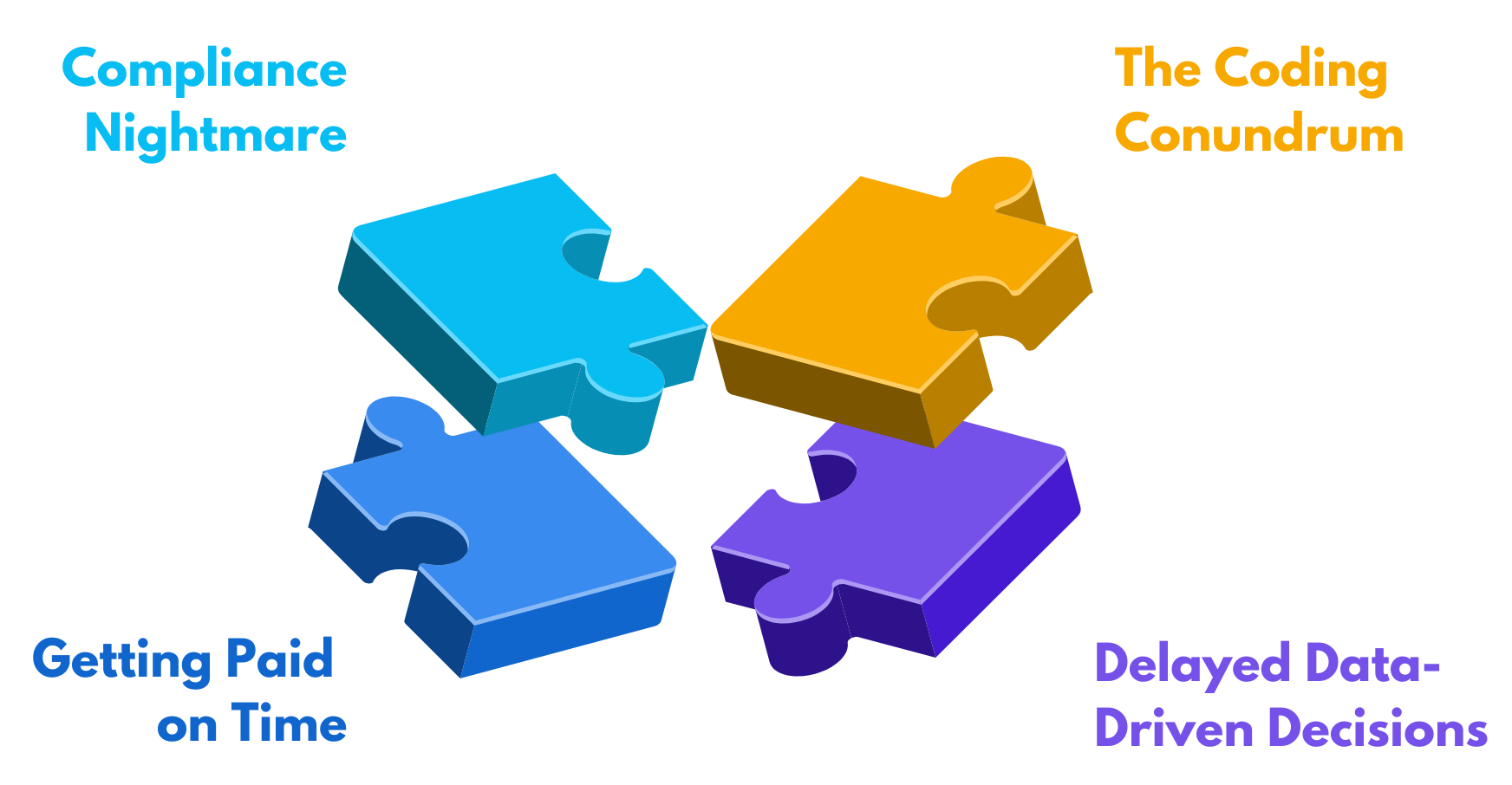
In today’s fast-evolving healthcare landscape, financial stability is just as critical as patient care — yet many providers are stuck navigating a revenue cycle filled with friction. From manual eligibility checks and coding errors to denied claims and delayed reimbursements, inefficiencies create a costly drain on time, revenue, and staff morale. In fact, nearly 90% of claim denials are preventable, yet providers continue to lose millions annually. It often feels like you’re leaving money on the table — and too often, that’s exactly what’s happening.
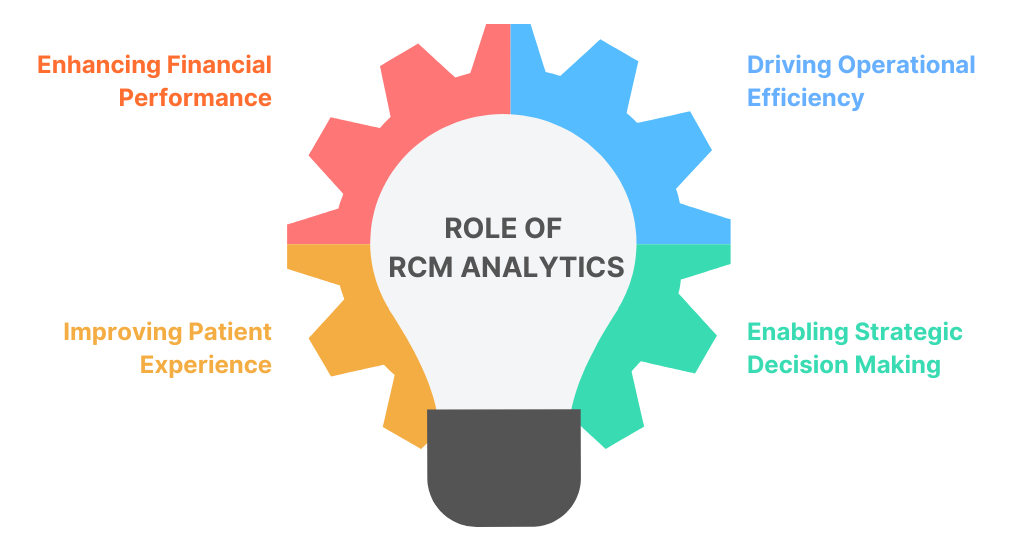
Enter Revenue Cycle Automation (RCA) — a strategic approach that redefines how healthcare organizations manage financial operations. By leveraging Robotic Process Automation (RPA) and intelligent workflow tools, RCA eliminates bottlenecks across the healthcare revenue cycle, driving greater speed, accuracy, and consistency in every transaction. The result? A more resilient, data-driven financial process built for today’s healthcare challenges.
What Can Be Automated in the Healthcare Revenue Cycle, and Why?
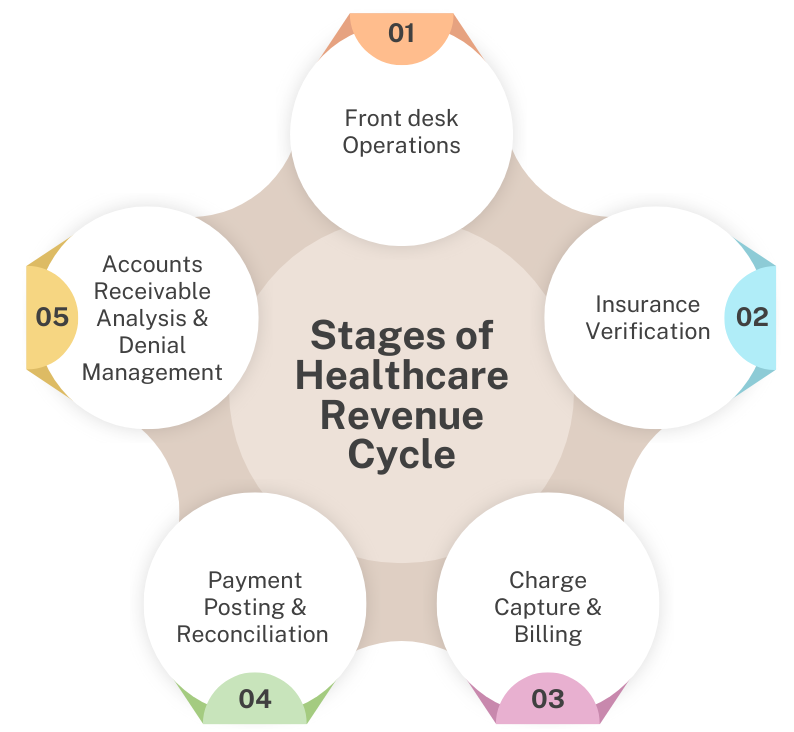
Every step in the healthcare revenue cycle has one thing in common: complexity. From patient registration to denial management, repetitive tasks and manual workflows create bottlenecks that delay payments and drain resources. But not every part needs a total overhaul. In fact, some of the most critical processes are also the easiest to automate. Here’s where providers can get the biggest wins with the least disruption.
Patient Scheduling and Registration
Accurate patient information at the scheduling and registration stage is critical to a healthy revenue cycle. Yet in many practices, this process is still handled manually — leading to incomplete forms, incorrect insurance details, and workflow bottlenecks that often snowball into denials and revenue loss.
So how does automation help here? By streamlining data entry, insurance verification, and digital form completion, providers can capture clean, validated data upfront. Information flows directly into systems with minimal human input, reducing errors and saving staff time. The result is a faster, more reliable intake process that supports both financial performance and a smoother patient experience.
Eligibility and Benefits Verification
Verifying a patient’s insurance coverage before the visit is one of the most crucial and time-consuming tasks in the revenue cycle. This is also a leading cause of downstream issues like claim denials, payment delays, and surprise bills. When done manually, the process can involve long phone calls, navigate payer portals, and deal with outdated or incomplete information.
This is where automation becomes indispensable. Automated eligibility and benefits verification, often powered by RPA, can run real-time checks with payers at the point of scheduling or registration. They instantly confirm coverage details, including co-pays, deductibles, and authorization requirements, flagging any potential issues immediately. The result is faster pre-visit workflows, fewer denials, and greater financial transparency for patients.
Coding and Charge Capture
Coding and charge capture form the critical link between services rendered and payments received. Yet, the sheer volume and complexity of codes, combined with manual workflows, often results in missed charges, underbilling, and compliance risks. Even small errors can trigger delays in payment or lead to costly audits.
Automation helps bring consistency and control to this process. Intelligent systems extract clinical data from EHRs, suggest CPT and ICD-10 codes, and validate them in real time. They can also detect uncaptured services and flag potential errors before submission. By ensuring every billable item is coded correctly and completely, automation helps maximize reimbursement, reduce audit risk, and safeguard revenue.
Claims Submission
You’ve done all the hard work – patient registered, benefits verified, codes captured. Now comes claims submission, where even minor slip-ups can cause major delays. Each payer has different rules, and one wrong field, a missing modifier, or an overlooked denial reason from a previous claim can kick things back into rework, slowing everything down.
With automation, claims get cleaner and faster. Claims are auto-scrubbed for errors, tailored to payer requirements, and submitted electronically, on time, every time. The result? Fewer rejections, faster acknowledgments, and end-to-end tracking that keeps your cash flow steady and your team focused.
Payment Posting
Receiving payments is a win but posting them accurately is where the real work begins. Manually processing Explanation of Benefits (EOBs) and Electronic Remittance Advices (ERAs) is a time-consuming, error-prone chore that can lead to misapplied funds, missed follow-ups, and revenue that quietly slips through the cracks.
Automated payment posting, powered by RPA and AI, instantly processes EOBs and ERAs, automatically applying payments, adjustments, and denials to the correct accounts, and flags discrepancies in real time. That means faster reconciliation, cleaner records, and a healthier cash flow with far less manual effort.
Denial Management
Claim denials are inevitable in the healthcare industry. However, letting them pile up is costly! Manually identifying, researching, and appealing each denied claim is a monumental task. This leads to a backlog that consumes significant staff time and leaves revenue uncovered.
Intelligent denial management tools, a key component of healthcare revenue cycle automation, can categorize denials by root cause, auto-route them for correction, and even trigger workflows to resubmit clean claims faster. This means faster resolution, higher appeal success rates, a dramatic reduction in manual rework, and a significant boost in the operational efficiency.
Common Misconceptions About Automating Revenue Cycle
We’ve seen how Revenue Cycle Automation can significantly streamline your operations. But it’s understandable that you might still have questions on whether this will actually work for you or not. We hear you! Despite its growing adoption, a few common myths still hold providers back. Let’s clear those up!
We’re not a big healthcare provider; this isn’t meant for us!
We hear you, and that’s totally fair. But the truth is, automation isn’t just for health systems with massive IT budgets. While there’s an initial investment, the ROI is quite substantial. Many tools are modular and built for practices of all sizes. You can pretty much start small and scale up without turning everything upside down. The cost savings from fewer errors, faster payments, and drastically improved efficiency typically far outweigh the implementation expense.
Will Automation Replace My Staff?
This is perhaps the biggest fear among many providers. The truth is automation will never replace your staff but empower them. How? By offloading repetitive, mundane tasks like endless data entry and routine verifications. Think of automation more as a digital assistant that lets your staff to focus on complex problem-solving, building patient relationships, and higher-value activities.
It Sounds Complicated!
“Won’t implementing automation be a nightmare for my practice?” We get it; bringing in new technology can instantly bring images of disrupted workflows and long staff training sessions. But modern RCA tools are designed with simplicity in mind. They integrate smoothly with your existing systems and start delivering value quickly, often without interrupting day-to-day operations.
That’s why working with the right partner makes all the difference. Reputable teams take a phased approach, integrating automation gradually into your existing workflows without flipping your operations upside down. This is exactly where VNB Health stands out. We specialize in Healthcare Revenue Cycle Automation that fits your pace and your priorities, helping providers start small, scale smart, and see real value early. Our team works collaboratively with you to identify high-impact opportunities, then implements automation step by step to ensure a smooth transition and continuous improvement.
Ready to Improve Your Revenue Cycle?
Healthcare revenue challenges aren’t going away — but how you handle them can change everything. The path to a healthier, more financially stable healthcare practice in today’s demanding environment isn’t about working harder, but smarter. While the challenges facing healthcare providers are significant, so are the opportunities for transformation. Eventually, automation is all about working smarter, reducing friction, and helping your people focus on what matters most – delivering exceptional care.
At VNB Health, we’re committed to making this transition seamless and impactful. We’re more than just a vendor; we are your strategic partner in this journey. Our phased approach and deep expertise in healthcare revenue cycles ensure that you gain efficiency from day one, with a clear roadmap for continuous growth.