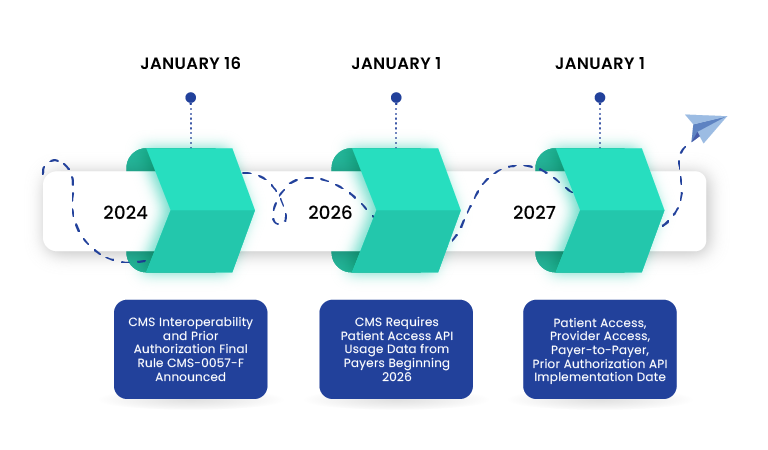
CMS-0057-F, officially known as the Interoperability and Prior Authorization Rule, aims to improve patient access to health information, streamline prior authorization processes, and enhance interoperability between healthcare systems. Centers for Medicare & Medicaid Services (CMS) released this rule in January 2024.
What does the rule impose?
The rule mandates healthcare stakeholders to adopt HL7 Fast Healthcare Interoperability Resources® (FHIR®) application programming interfaces (APIs). By standardizing data exchange between healthcare systems, this initiative aims to:
- Streamline Prior Authorizations: Accelerate approval processes for treatments and medications
- Enhance Data Exchange: Facilitate seamless information sharing between healthcare providers
- Improve Patient Access: Empower patients with greater control over their health information
This means doctors, hospitals, and insurance companies have to use a specific technology to quickly and securely share patient data. Thus, making healthcare more efficient and patient centered.
Who Does CMS-0057-F Apply To?
The rule applies to a broad range of healthcare entities and professionals involved in the provision of care to Medicare beneficiaries, as well as those involved in the administration of Medicare benefits. Specifically,
- Healthcare Providers such as Hospitals, clinics, physician practices
- Medicare Advantage [MA] Organizations, State Medicaid and Children’s Health Insurance Program [CHIP] agencies, Medicaid managed care plans and CHIP managed care entities, Qualified Health Plan [QHP] issuers on Federally Facilitated Exchanges [FFEs])
Key Deadlines for CMS-0057-F Compliance
To avoid financial penalties and operational disruptions, healthcare organizations must meet these key deadlines:
January 1, 2026 – Payers must implement critical operational provisions like shortened prior authorization timelines and public reporting requirements
January 1, 2027 – Payers must fully implement FHIR-based APIs for patient access, provider access, and payer-to-payer data exchange.
Why is CMS-0057-F Important for Healthcare Providers and Payers?
Let’s break it down. Imagine you’re a patient, and you need to switch doctors or hospitals. With the Interoperability and Prior Authorization Rule in place, your medical records can easily move with you, no more lost paperwork or frustrating delays.
For healthcare providers, this rule means less paperwork and more time to focus on patient care. No more endless forms and phone calls to get prior authorizations. It’s like having a digital assistant that handles all the stuff!
And for health insurance companies, it’s about efficiency. By streamlining processes and improving data exchange, they can save money and better serve their members.
So, whether you’re a patient, a doctor, or an insurance company, the Interoperability and Prior Authorization Rule is a step towards a more connected, efficient, and patient-centered healthcare system.
Key Objectives of CMS-00570F
In summary, CMS-0057-F introduces 4 key technical elements to modernize healthcare. These elements, primarily focused on prior authorizations and payer interactions, aim to enhance data exchange and interoperability. By streamlining information flow between payers, providers, and patients, this initiative lays the groundwork for a more efficient and patient-centric healthcare system.
Patient Access API
CMS-0057-F expands the scope of the Patient Access API, originally introduced in CMS-9115-F. This HL7 FHIR-based API now requires payers to share additional information with members. Specifically, payers must provide updates on prior authorization status (excluding drug-related ones). Payers must report the API utilization metrics to CMS from January 1, 2026.
Provider Access API
Payers are now required to share patient data with in-network providers who request it, as long as the patient hasn’t opted out. This data will be shared through a FHIR-based Provider Access API and will include information about prior authorizations, including individual claims and encounter data. Plus, payers have to explain to patients in easy-to-understand language why sharing data with their doctors through these APIs is a good thing, and that they can choose not to share their data if they want to.
Payer-to-Payer API
Payers must implement and maintain a Payer-to-Payer API that will facilitate health plans share data to ensure smooth transitions for patients switching plans or with multiple coverages. Payers must share critical information such as claims, encounter data, and prior authorization details when a patient opts-in for this. They must obtain explicit consent from individuals before sharing their data. When the patient switches to a new payer, they can request up to five years of historical data from the previous payer.
Prior Authorization API
Payers must implement and maintain the Prior Authorization API that will streamline the prior authorization process by providing a standardized way for healthcare providers to submit requests and receive decisions from payers. This facilitates the electronic exchange of information such as covered services, documentation requirements, and approval or denial statuses.
New deadlines for Prior Authorization Decisions
Prior Authorization Decision Timeframes – For urgent requests, Payers must send their decisions within 72 hours and for normal requests within seven calendar days, irrespective of how the request comes to them (fax/email/electronic format/etc.,) Starting 2026, Payers should also provide a specific reason for denied decisions, if any.
Prior Authorization Metrics – Starting January 1, 2026, Payers must publicly report certain prior authorization metrics every year on their website.
Key Steps for Payers & Providers to Comply with CMS-0057-F
| Key Steps | Payers | Providers |
|---|---|---|
| Technology Investment | Invest in robust technology infrastructure (such as EHR systems, data exchange platforms) to support FHIR-based data exchange and ensure data security. | Implement EHR systems that can integrate with payer systems to facilitate data exchange. |
| Process/Workflow Optimization | Streamline prior authorization and claims processing workflows. | Streamline clinical workflows. |
| Interoperability | Develop and maintain FHIR-compliant APIs to enable seamless data exchange with providers and other payers. | Utilize EHR systems and other technologies to facilitate data exchange and interoperability with Payers. |
| Training | Payers must educate patients, providers, and internal staff about the new data sharing options and how to utilize them effectively. | Providers must train staff on how to use new technologies and data exchange processes to maximize their effectiveness. |
Impact of CMS-0057-F on the Healthcare Landscape
By standardizing data exchange, CMS-0057-F is poised to drive significant improvements in the healthcare industry. As the healthcare industry continues to evolve, by embracing this rule and its underlying principles, healthcare organizations can position themselves for long-term success.
Improved Patient Outcomes – Enhanced data sharing can lead to more informed clinical decisions, better care coordination, and ultimately, improved patient outcomes.
Increased Operational Efficiency – Streamlined processes, reduced administrative burdens, and faster claims processing can lead to significant cost savings for healthcare organizations.
Enhanced Patient Experience – Patients will benefit from easier access to their health information, quicker prior authorization approvals, and a more seamless healthcare experience.
Innovation and Digital Health – Standardized data exchange can accelerate the development and adoption of innovative digital health solutions.
What’s Next?
Navigating the complexities of CMS-0057-F can be daunting. But it doesn’t have to be. By embracing interoperability, healthcare organizations can streamline operations, improve patient care, and reduce costs. VNB Health is your partner in this journey.
So how can VNB Health help you achieve compliance and optimize your workflows?
FHIR Implementation:
- Simplify your healthcare data exchange with our expert FHIR implementation services.
- Ensure seamless integration with your existing systems, reducing errors and saving time.
Data Standardization:
- Transform your healthcare data into a powerful asset with our data standardization services.
- Streamline your data, improve accuracy, and enhance decision-making.
Workflow Optimization:
- Analyze your existing workflows and identify areas for improvement.
- Leverage FHIR and standardized data to streamline your processes, boost productivity, and reduce administrative burdens.
Ready to take the next step? Contact us today for a free consultation. Also visit our in-depth resource page on CMS Interoperability, Patient Access, and Prior Authorization to see how we can help you stay ahead of the curve.
Wrapping Up
CMS-0057-F throws a whole new set of acronyms and deadlines at you. Sure enough, we understand that! But hear us out – with a little preparation, this rule can actually be a game-changer for how you handle prior authorizations. Think faster approvals, smoother workflows, and a happier healthcare experience for everyone.
Remember, 2027 is coming (slowly, but surely) and the key is to start early! Get your IT crew, compliance team, and whoever else needs a heads-up involved now. Let’s work together to make this transition smooth and unlock the future of connected healthcare!